Domestic and sexual violence rates much higher among people with severe mental illness
A 2014 study from the United Kingdom shows stark differences in the occurrence and consequences of domestic and sexual violence victimization in the adult lives of people with severe mental illness (SMI), compared to the general population. Severe mental illness was defined in this study as having mental disorders that qualify them for having designated caseworkers from state health services. The researchers were able to survey a random sample of almost 300 people with SMI for the study, and the comparison with the general population came from a nationally representative sample of over 22,000 people.
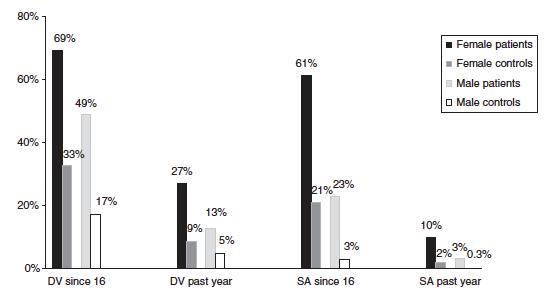
You can see in the chart below the differences between rates for people with SMI (patients) and for the general population (controls). The study looked at how many people had experienced domestic violence and sexual assault since they were 16 years old, as well as in the past year alone.
Among people who had experienced severe sexual assault (SSA), which the study defined as nonconsensual penetration or oral sex, people with SMI were also more likely to experience many kinds of negative effects than the general population. People with SMI were significantly more likely to have mental or emotional problems, difficulty sleeping, depression, mistrust of others, stopping going out, and attempting suicide. They were also more likely to have physical injuries from bruises to broken bones, pregnancy, and sexually transmitted infections, but this difference was not statistically significant.
Just to give you a clearer picture of what these consequences looked like, 91.8% of people with SMI had adverse psychological consequences after SSA, as compared to 64.2% of the general population. And 53.1% of these people with SMI attempted suicide as a result of SSA, as opposed to 3.4% of the general population.
What does this mean for prevention? Though this information came from Britain, it is probably safe to assume that there are similar trends in the United States. People with SMI appear to be extremely vulnerable to sexual and domestic violence, and they also have higher rates of severe health problems after SSA. First of all, we need more research about the special risk and protective factors for this population, so we know more about how to prevent sexual and domestic violence against them. Once we know more, some primary prevention efforts should clearly be targeted toward people who live with, care for, and regularly interact with people with SMI.
Full citation: Khalifeh, K. et al. (2014). Domestic and sexual violence against patients with severe mental illness. Psychological Medicine. Advance online publication. doi:10.1017/S0033291714001962
Link to full article (free): http://journals.cambridge.org/download.php?file=%2FPSM%2FS0033291714001962a.pdf&code=a1d706d3812b8bb7e6bbfbf916a408e1
Full abstract:
Background. Domestic and sexual violence are significant public health problems but little is known about the extent to which men and women with severe mental illness (SMI) are at risk compared with the general population. We aimed to compare the prevalence and impact of violence against SMI patients and the general population.
Method. Three hundred and three randomly recruited psychiatric patients, in contact with community services for 51 year, were interviewed using the British Crime Survey domestic/sexual violence questionnaire. Prevalence and correlates of violence in this sample were compared with those from 22606 general population controls participating in the contemporaneous 2011/12 national crime survey.
Results. Past-year domestic violence was reported by 27% v. 9% of SMI and control women, respectively [odds ratio (OR) adjusted for socio-demographics, aOR 2.7, 95% confidence interval (CI) 1.7–4.0], and by 13% v. 5% of SMI and control men, respectively (aOR 1.6, 95% CI 1.0–2.8). Past-year sexual violence was reported by 10% v. 2.0% of SMI and control women respectively (aOR 2.9, 95% CI 1.4–5.8). Family (non-partner) violence comprised a greater proportion of overall domestic violence among SMI than control victims (63% v. 35%, p<0.01). Adulthood serious sexual assault led to attempted suicide more often among SMI than control female victims (53% v. 3.4%, p<0.001).
Conclusions. Compared to the general population, patients with SMI are at substantially increased risk of domestic and sexual violence, with a relative excess of family violence and adverse health impact following victimization. Psychiatric services, and public health and criminal justice policies, need to address domestic and sexual violence in this at-risk group.
